Protein often gets side-eyed in recovery spaces – dismissed as diet culture, a fad, or worse, “ED in disguise.” But anorexia isn’t just fat loss. It’s body-breaking. Recovery is bodybuilding. Protein isn’t a trend – it’s the raw material for repairing your heart, bones, and brain.
In this post, I’m going to tackle some of the biggest myths about protein in recovery, with science where it fits. For context, every single one of these myths came from just one day of scrolling Recovery TikTok – some even from professionals. That’s how widespread these misconceptions are.
And if you’ve ever wondered why everyone suddenly seems “obsessed with protein,” this post might give you some clarity.
As this is a long post, here’s the table of contents.
- Biology Myths
- Recovery Myths
- General Protein Myths
- Recovery IS Bodybuilding Thats Why I Eat Like A Gym Bro
- Final Thoughts
- References
Biology Myths
Myth: “You only need protein if you’re protein deficient.”
Truth: That’s like saying you only need water if you’re dehydrated. Protein isn’t some emergency supplement – it’s a macronutrient. Your body needs it every single day to keep you functioning.
Bones? Built on a protein matrix.
Muscles? Literally protein fibers.
Your heart? A muscle. It shrinks during starvation.
Even your immune system and enzymes depend on protein.
If you’ve had anorexia, you are protein deficient by definition – your body broke down muscle, heart, and organ tissue to survive. That doesn’t magically rebuild on a low-protein diet.
Myth: “You don’t need protein because overshoot fat magically heals your lean mass.”
Truth: Fat does not “convert” into lean mass. Fat is fat. Muscle is muscle. They’re different tissues with different repair needs. Fat doesn’t “heal” you – not in the way it’s represented, anyway.
What fat overshoot actually means is that your body is storing extra energy in case you starve it again. Whilst that fat is crucial it doesn’t sneak off in the night to rebuild your bones or heart. Food you eat everyday does – specifically, amino acids from protein combined with energy from carbs and fat.
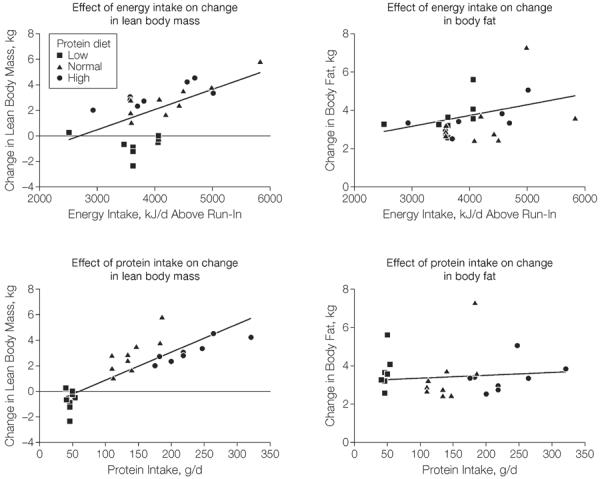
Modern DXA studies back this up: in overfeeding studies, fat always comes back faster than lean tissue. And the higher the calorie surplus, the more disproportionate fat you gain compared to lean mass if you only eat the bare minimum protein. This even happens in healthy-weight people at their set point – people who don’t have anything to “heal.” No one calls that “magical healing fat.”
Overfeeding studies also show that low protein diets = more fat overshoot, high protein diets = more lean tissue gained (source). That’s without exercise. So no, fat overshoot doesn’t magically heal you – if anything, protein determines how much of that surplus goes into repair of lean mass versus just storage.
Advocates of “magical healing fat” often point to the Minnesota Starvation Study as proof. Yes, those men regained lean mass – but remember:
– They were young, healthy men with testosterone rebounds. You cannot compare women to men who can gain lean mass more easily.
– It was the 1940s – no DXA scans, just crude weight and circumference measures.
– They didn’t have a history of ED or years of malnutrition before the study. So they wouldn’t have lost as much lean mass as someone with a long history of restriction. They were only put on a calorie deficit for 24 weeks, not years.
– The calorie deficit they were on, while enough to cause them to lose significant bodyweight was not as extreme as the calorie deficit of someone with a severe eating disorder.
And here’s what almost no one mentions: many women with anorexia also have hypothalamic amenorrhea (HA). HA isn’t just “missing your period” – it means low estrogen, which directly worsens lean mass loss (source). Estrogen normally helps protect both muscle and bone. Without it, bone breakdown accelerates and muscle preservation weakens.
So if women with HA had been in Minnesota? Their lean mass losses would’ve been worse than the men’s. And fat overshoot alone wouldn’t repair that damage, because lean mass recovery needs two things:
– Enough protein (to rebuild tissue), and
– The return of estrogen (to normalise bone and muscle turnover).
Modern data shows this clearly: a 27-year follow-up study of women who had recovered from anorexia still found significantly lower bone density and muscle strength than controls. If fat overshoot really “magically” turned into lean mass, that gap wouldn’t exist.
If I was still relying on technology from the 1940s I’d be writing this on Charles Babbage’s analytical machine, not a MacBook Pro – but apparently it’s fine to rely on outdated science when people’s long-term health is involved.
Lean mass can rebuild, but only if you give your body the raw materials. And that means enough complete protein, every single day.
Recovery Myths
Myth: “You’re trying to gain muscle and not fat. That’s why you’re eating protein”
Truth: Gaining fat is crucial to recovery – but so is lean mass. And the reality is, bodies almost always gain muscle and fat together. The only exception is if you already have a much higher body fat percentage (around 30%) where you can lose fat and gain muscle at the same time. Again though, the fat doesn’t “turn into” muscle.
When you’re lean and you gain weight – even if you’re eating protein and lifting in the gym specifically to build muscle – you will always gain fat alongside lean mass (source). Fitness people know this too: it’s why “bulking” is always followed by “cutting.” They bulk to build muscle, then cut to lose the fat that inevitably and unavoidably came with it.
Bodybuilding would be a heck of a lot easier if you could only gain muscle and not fat. But then they also wouldn’t be posting those day after competition cheat day videos which I know for a fact most of you have watched if you have had anorexia.
So no, eating protein in recovery isn’t about “avoiding fat gain.” That’s literally impossible. Your body will naturally put on fat for organ protection and as insurance in case you starve it again. At the same time, if you eat enough protein, it will rebuild lean mass too. Both are necessary but recovery spaces only ever focus on one, and don’t mention the other.
Myth: “You have to gain fat first before you can gain muscle.”
Truth: Not true. In fact, you’ll usually gain more lean mass during weight restoration than at any other stage. Waiting until after to “start building muscle” is a missed opportunity.
When you’re underweight, your body enters a unique anabolic state. Think of it like “repair mode on steroids” (pun intended but I’m still natty):
– Muscle & bone are hypersensitive – they respond faster to protein and calories than when you’re weight restored.
– Nutrient partitioning shifts – instead of shuttling most energy into fat storage, your body prioritises rebuilding lean tissue if enough protein is ingested (muscle, organs, bone).
– It won’t last forever – once you reach your set weight, muscle-building becomes like normal bodybuilding: slower, harder, and usually requiring extra surplus. (source)
Basically If you wait until you’re at your “set weight,” you’re often left with disproportionate fat gain and lower lean mass. That actually makes muscle-building harder later, because you’re not just repairing – you’d need to “bulk” on top of your set weight to drive muscle growth.
And honestly? That’s not just inefficient, it’s mentally brutal. Imagine hitting your set weight, thinking you’re “done,” and then being told you now need to eat in surplus again and gain more weight to build muscle, lean mass and bone. For most people in recovery, that’s a nightmare scenario.
The good news is: your body will build fat and lean mass together during weight restoration, if you give it what it needs – enough food, and enough protein. You don’t need to gain fat first. You need to fuel the whole rebuilding process as it happens.
Myth: “You’re just trying to fill up on protein so you eat less in recovery.”
Truth: Protein doesn’t magically kill extreme hunger. I kind of wish it did, so I didn’t end up fist-deep in a jar of Biscoff spread as much as I did – but it really doesn’t. The only time protein seems to help is when my body actually needed protein, but it asked for something else.
In recovery, especially from malnutrition, bodies crave fast carbs and fat. They don’t usually scream “eggs and chicken breast.” But sometimes the body’s really hunting for protein and tries to get it inefficiently through carbs and fat.
To hit 40g of protein (what I aim for per meal), I’d need to eat:
– 500g of Fruit & Fibre cereal, or
– 150g of peanut butter.
So maybe that’s why sometimes I’ve craved a whole box of cereal or a full jar of peanut butter. Bodies in recovery are unreliable translators – cravings don’t always map directly to what’s missing. Just like bodies that are anaemic often craving ice or non food items.
Myth: “Eating protein bars in recovery is just another ED in disguise.”
This one really gets to me, because it’s almost always said by someone who claims to be in recovery themselves – and yet takes it upon themselves to judge other people for posting that they ate a protein bar. If you’ve lived with an ED, you should know how toxic and damaging it is to comment on someone else’s food choices, especially when they’re vulnerable in recovery.
Refusing to eat an entire food group, demonising it, and shaming others for eating it? That’s ED behaviour, not recovery behaviour. And slapping “ED in disguise” on a protein bar is absurd. You don’t even know why someone is eating it.
What if they have blood sugar issues, which are common in recovery? What if they have other medical needs or dietary restrictions? Protein bars let me eat something chocolatey without crashing into reactive hypoglycaemia. To dismiss that as “disordered” is not just ignorant, it’s ableist.
And let’s be clear: labelling anyone who eats a protein bar or touches a weight as orthorexic is stigmatising and minimises what orthorexia actually is. Orthorexia is a serious, life-limiting eating disorder. It is not “having a Barebells bar once a day.”
Yes, people can swap one disorder for another. But even if it was true, when it’s mostly an overblown exaggeration to a Barebells bar, how does piling shame onto someone for eating a protein bar help them? Maybe instead, ask yourself why you’re demonising an entire macronutrient.
And let’s be real – context matters, even though no one seems to care about it online. A protein bar eaten in the car as part of a high-carb, balanced day is not orthorexia – it’s practicality. Recovery isn’t ruined by one bar. But shaming someone for it? That’s ED logic disguised as recovery advice.
General Protein Myths
Myth: “It’s not protein you should care about, it’s fibre – people are dying of colon cancer.”
Truth: I don’t know anyone who cares about protein that doesn’t also care about fibre. In fact, if you ate nothing but protein with zero fibre, you’d have… let’s just say catastrophic relationship ending bathroom issues.
The reality is, high-protein diets almost always come with plenty of fibre. My protein bars, for example, have 12g of fibre each – that’s the same as three 40g bowls of Fruit & Fibre cereal. Except instead of eating three bowls of cardboard, I get it in one snack.

Protein and fibre aren’t enemies. If anything, they show up together more often than not (by the way, I’m writing this while eating a kiwi with the skin on).
Myth: “Making sure you get enough protein is diet culture.”
Truth: No, it isn’t. The same way making sure I get enough carbs, fat, or fibre isn’t diet culture. I track all of those too.
Is protein trendy right now? Yes.
Are corporations slapping “high protein” on anything they can to cash in? Also yes.
Case in point: I buy “protein balls” from Lidl. They’re higher in fat and carbs than protein. A few years ago they would’ve been called “energy balls.” Now they’ve been rebranded with a price premium because nobody would buy them if they were honestly called what they are: fat balls. (Well – except me, because I like fat and they taste amazing. And I’m too asexual to be deterred by the innuendo.)
Here’s why protein is everywhere right now:
– Science has pushed protein into the spotlight, especially with Ozempic and other weight-loss drugs. Doctors recommend higher protein on those meds. (source)
– Corporations saw the pound signs and rolled out whole protein product lines.
– Walmart in the US literally lost money because people on Ozempic bought fewer total units of food. So companies needed to make it back – hence the sudden flood of “protein” products.
That’s great news for me, for bodybuilders, and for anyone who cares about eating enough protein. I don’t have to trudge to a health food shop and pay premium prices – Lidl sells it now. Just because corporations seem to want us to eat it, doesn’t mean it’s always wrong or diet culture.
Recovery IS Bodybuilding Thats Why I Eat Like A Gym Bro
Getting enough protein in recovery isn’t about changing what you see in the mirror, it’s about repairing parts of your body that you can’t see. Lean mass isn’t just muscle – it’s your bones, heart, kidneys, digestive system. All of these need repair, and your body cannot rebuild them without daily amino acids from complete protein sources.
Bones aren’t just “calcium sticks” – they’re built on a protein matrix and need more than just milk and cheese. Your heart is literally a muscle. And fat mass doesn’t magically heal damage done to them through malnutrition. Without adequate protein, your body will only patch the bare minimum.

That’s exactly what happened to me last time when I did All In. I regained all the weight to my set point, but I still had visible muscle atrophy. I gained disproportionate fat compared to lean mass. I even liked it at the time, because it made me look slight and stringy – but the trade-off was weakness, chronic pain, fatigue, and mobility issues. If I could still see atrophy in my thighs and forearms, what state were the parts I couldn’t see in? My heart? My bones? And sure enough, the research shows it: women with anorexia still have lower lean mass than controls even 27 years into recovery.
For women especially, lean mass takes consistent effort to rebuild. The Minnesota men had testosterone rebounds and were studied with 1940s methods – you can’t compare that.
Past the age of 35 too, anabolic resistance kicks in, which means you need more protein just to build the same amount of lean mass as when you were younger. I’m 41, and I learned the hard way: fat doesn’t magically turn into lean mass with age. Instead, I lost what little lean mass I had, gained even more fat, and my mobility and pain got worse. Less movement > less bone stimulus > even weaker foundation. And yet in All In recovery you’re told: don’t move, don’t think about macros. That’s a recipe for not rebuilding lean mass but the bare minimum.
We don’t have long-term studies on people who’ve gone All In, but we do have plenty of overfeeding studies – and they show disproportionate fat gain every time. Add in the current trend of avoiding protein as “diet culture,” and the outcome doesn’t look good.
That’s why I had to write this. I don’t want anyone ending up where I was: 40 years old, in pain, weak, and feeling older than I am because of years of low lean mass because someone said “All in” was the only right way to recover. They said that magical healing fat would take care of the rest. It didn’t. Things only got worse despite my commitment to recovery.
In recovery, you’re rebuilding far more than a bodybuilder ever is – which is exactly why I eat like one. The WHO and NHS guidelines of 0.8 g of protein per kilo of bodyweight are set far too low for that purpose (source). They were designed for healthy people eating just enough to avoid losing muscle and function, not for people who need to rebuild what’s been lost.
When you’re trying to build lean mass, the evidence-based recommendations sit much higher – around 1.6–2.2 g of protein per kilo of bodyweight (source). Since the start of my recovery, I’ve been aiming for the upper end, around 2 g per kilo, because that’s what actually supports the amount of muscle and bone rebuilding I need to do.
Final Thoughts
Protein isn’t diet culture. It’s not a fad. It’s survival. In recovery, fat gain matters and is crucial – but so does rebuilding the lean mass that keeps you alive and moving. Bones, muscles, organs, your heart – they don’t repair themselves on wishful thinking or magical healing fat. They repair with food, and especially with protein. Recovery is bodybuilding, whether you like the sound of it or not.
I’m not here to tell you what to do. Or to judge anyone else for doing what they have to, recovery is different for everyone. But untruths never helped me in recovery so I’m here to dispel myths and explain why I’ve made the choices I have in recovery. Protein for me, has been the difference between rebuilding properly and repeating the same mistakes I made last time.
I also don’t blame or judge anyone for believing in magical healing fat, it can feel cult like in the recovery community. I even believed in it last time I recovered without questioning it and I have always been logical and loved science. It’s very persuasive, prevalent and everyone that doesn’t follow it gets judged for “not recovering the right way”.
Recovery advice, like any form of healthcare, should be based on best interests and informed consent. But how can you know if something’s in your best interests – or truly give informed consent – if the information you’re given isn’t factual?
There will be more posts where I go into my personal experience of high protein recovery – before and after, weight differences, and compared to when I went All In. For now, just know: I’m sharing this because I don’t want anyone else left confused by the noise out there. Lies aren’t comfort, comfort comes from knowing what’s real and being validated. Recovery from a mental illness requires a commitment to reality.
References
Biology Myth References
Bray GA et al., 2012 (JAMA) – Effect of dietary protein on weight gain, energy expenditure, and body composition during overeating in healthy adults. https://pubmed.ncbi.nlm.nih.gov/22215165 8 weeks of overfeeding (+40% calories). Low protein – almost all fat gain. Normal/high protein – more lean mass gained even without exercise.
Misra M & Klibanski A, 2014 (Endocrine Reviews) – Bone health in anorexia nervosa. https://pubmed.ncbi.nlm.nih.gov/24731664 – Shows protein + IGF-1 + estrogen interplay in lean tissue and bone recovery.
Reduced Bone Strength and Muscle Force in Women 27 Years After Anorexia Nervosa – Sandro Manuel Mueller, Marilyn Immoos, Elmar Anliker, Suzana Drobnjak, Urs Boutellier, Marco Toigo https://academic.oup.com/jcem/article-abstract/100/8/2927/2836105?redirectedFrom=fulltext
Recovery Myth References
The Effects of Overfeeding on Body Composition: The Role of Macronutrient Composition – A Narrative Review – Alex Leaf Jose Antonio https://pmc.ncbi.nlm.nih.gov/articles/PMC5786199 (If you read any of these, read this one, it combines multiple overfeeding studies, all of which prove high protein in overfeeding is more preferable to lean mass gains like this example –
Overfeeding with Low protein (0.7 g/kg):
+3.7 kg weight
+3.1 fat, –0.7 lean – 119% fat gain
Overfeeding with High protein (2.4 g/kg), 1000-calorie surplus, sedentary:
+2.2 kg weight
+1.1 fat, +1.1 lean – 50/50 fat to lean
Catabolic to anabolic transition during nutritional rehabilitation of female adolescents with anorexia nervosa – Yael Levy-Shraga, Idit Ron, Adi Enoch-Levy, Rina Hemi, Hannah Kanety, Ido Wolf. https://journals.physiology.org/doi/full/10.1152/ajpendo.00523.2024?
Recovery is Bodybuilding references
Is It Time to Reconsider the U.S. Recommendations for Dietary Protein and Amino Acid Intake? Mary Weiler, Steven R Hertzler, Svyatoslav Dvoretskiy – https://pmc.ncbi.nlm.nih.gov/articles/PMC9963165
Dietary Protein and Muscle Mass: Translating Science to Application and Health Benefit. John W Carbone, Stefan M Pasiakos – https://pmc.ncbi.nlm.nih.gov/articles/PMC6566799
